Claims Denials and Appeals in ACA Marketplace Plans in 2023 | KFF
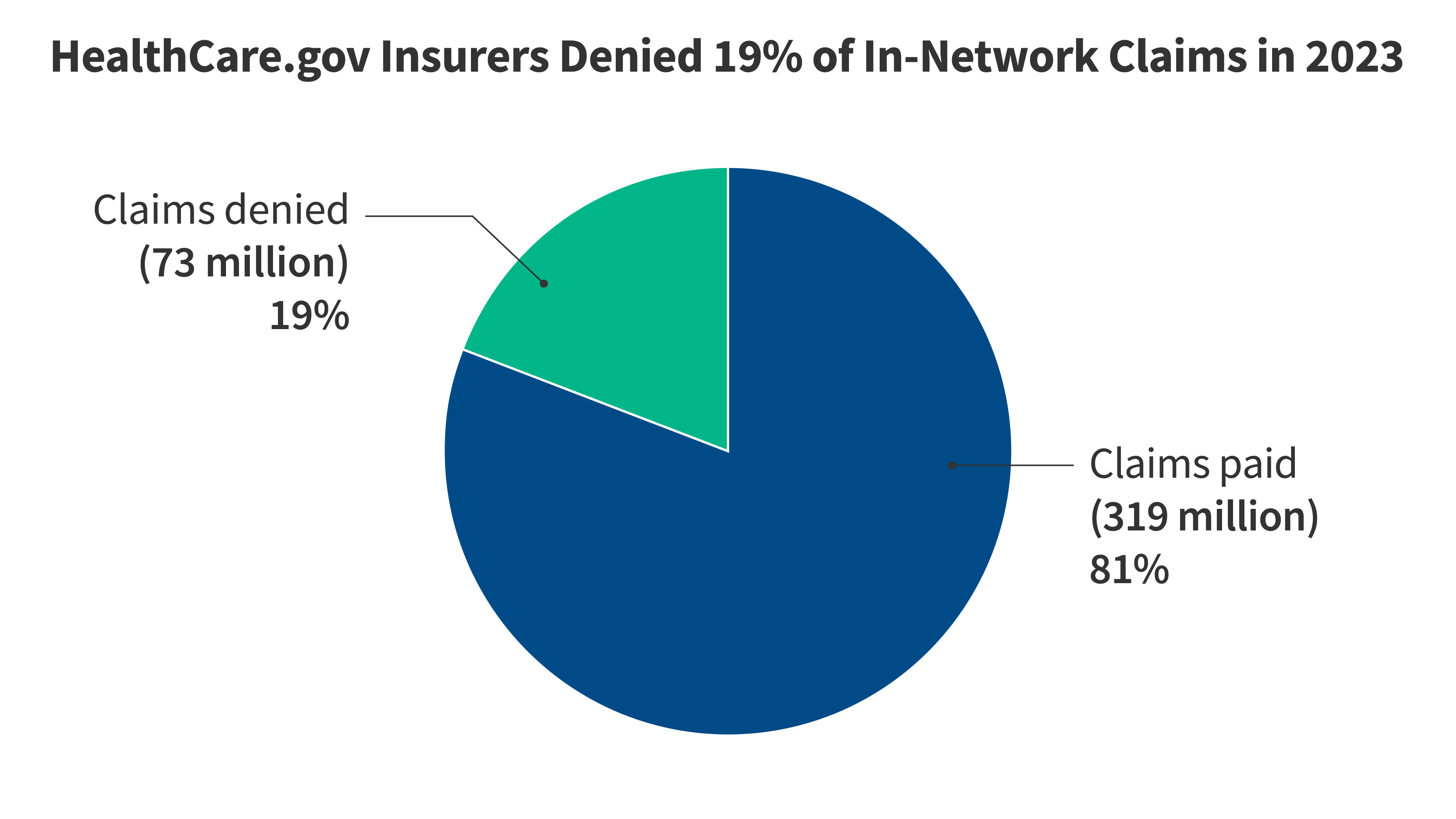
This brief analyzes federal transparency data released by the Centers for Medicare and Medicaid Services (CMS) on claims denials and appeals for non-group qualified health plans (QHPs) offered on HealthCare.gov in 2023. It finds that HealthCare.gov insurers denied nearly one out of every five claims (19%) submitted for in-network services. Information about the reasons for denials is limited, and few consumers appeal claims denials.| KFF