CMS finalizes rule tightening prior authorization turnaround for insurers | Healthcare Dive
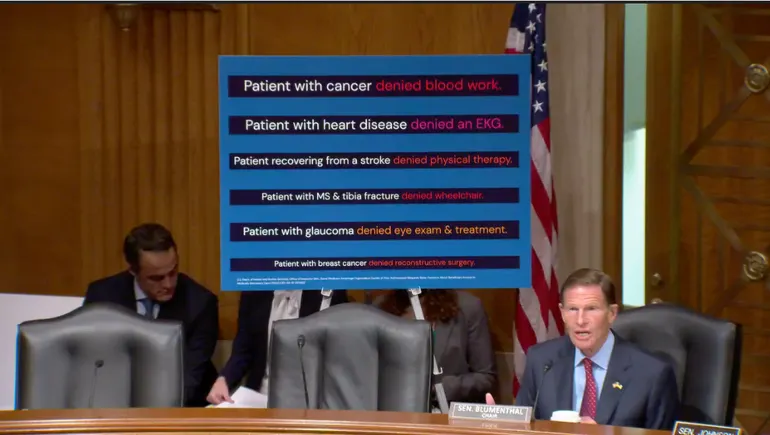
Payers have new deadlines to issue prior authorization decisions — 72 hours for urgent requests and seven days for non-urgent ones — that should cut back coverage determination limbo for patients.| Healthcare Dive